Clinician Scientific & Educational Resources
-
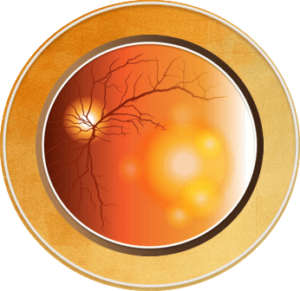
If AMD does progress to the wet stage, therapies such as injections and laser treatments can help.
-
Vision loss may be rapid and severe. Patients may see a dark spot (or spots) in the center of their vision due to blood or fluid under the macula.
-
Straight lines may look wavy because the macula is no longer smooth. Side or “peripheral” vision is rarely affected; however, some patients do not notice any such changes, despite the onset of neovascularization. Therefore, periodic eye examinations are very important for patients at high risk.

 Go 6th slide
Go 6th slide
An Introduction to Age-related Macular Degeneration
Age-related macular degeneration (AMD) is a major cause of blindness worldwide and is the leading cause of vision loss and blindness for Americans aged 65 years and older. The number of older Americans is projected to nearly double from 48 million to 88 million in 2050.1
AMD is clinically classified as early-stage (medium-sized drusen and retinal pigmentary changes) to late-stage (neovascular and atrophic). Described as a multifactorial disorder, dysregulation of the complement, lipid, angiogenic, inflammatory, and extracellular matrix pathways has been implicated in its pathogenesis. Future progress is likely to be from improved efforts in prevention and risk-factor modification, personalized medicine targeting specific pathways, anti-vascular endothelial growth factor agents or other agents, and regenerative therapies.2
There are two basic types of AMD: “wet” and “dry” with approximately 10%-15% of cases of AMD being the “wet” or exudative type (neovascular). With “wet” AMD, abnormal blood vessels, called choroidal neovascularization (CNV), grow under the retina and macula. These new blood vessels may then bleed and leak fluid, causing the macula to bulge or lift up from its normally flat position (macular edema), thus distorting or destroying central vision. Under these circumstances, vision loss may be rapid and severe. Patients may see a dark spot (or spots) in the center of their vision due to blood or fluid under the macula. Straight lines may look wavy because the macula is no longer smooth. Side or “peripheral” vision is rarely affected, but it is important to recognize that some patients do not notice any such changes, despite the onset of neovascularization; therefore, periodic eye examinations are very important for patients at high risk.1,3,4
Age-related Macular Degeneration in the United States5
- By 2050, the estimated number of people with AMD is expected to more than double from 2.07 million (in 2010) to 5.44 million
- The majority of AMD cases occur among white Americans; however, Hispanic Americans will see the greatest rate of increase, with a nearly six-fold rise in the number of expected cases from 2010 to 2050
- Women generally have a longer life expectancy than men and are, therefore, more likely to develop age-related eye diseases such as AMD
In this Clinical Toolkit, you will find recent treatment recommendations and information on current and emerging therapies that impact treatment selection. A list of additional resources is provided to help improve the clinical outcomes of patients with AMD. Read more about the symptoms of wet and dry AMD with our clinician educational resources.
References
- Centers for Disease Control and Prevention (CDC). Learn About Age-Related Macular Degeneration. https://www.cdc.gov/features/healthyvisionmonth/index.html. Accessed March 6, 2020.
- Mitchell P, Liew G, Gopinath B, Wong TY. Age-related macular degeneration. Lancet. 2018;392(10153):1147-1159.
- American Macular Degeneration Foundation [AMDF website]. Wet Macular Degeneration. https://www.macular.org/wet-amd. Accessed March 6, 2020.
- Fine AM. Earliest symptoms caused by neovascular membranes in the macular. Arch Ophthal. 1986;104:513-514.
- National Institutes of Health (NIH)/National Eye Institute (NEI). AMD Data and Statistics. https://www.nei.nih.gov/learn-about-eye-health/resources-for-health-educators/eye-health-data-and-statistics/age-related-macular-degeneration-amd-data-and-statistics. Accessed April 1, 2020.