Diagnosis and Associated Risk Factors
When evaluating a patient who shows signs and symptoms that suggest age-related macular degeneration (AMD), it is important to conduct a comprehensive adult medical eye evaluation, paying special attention to those aspects that are relevant to AMD.1
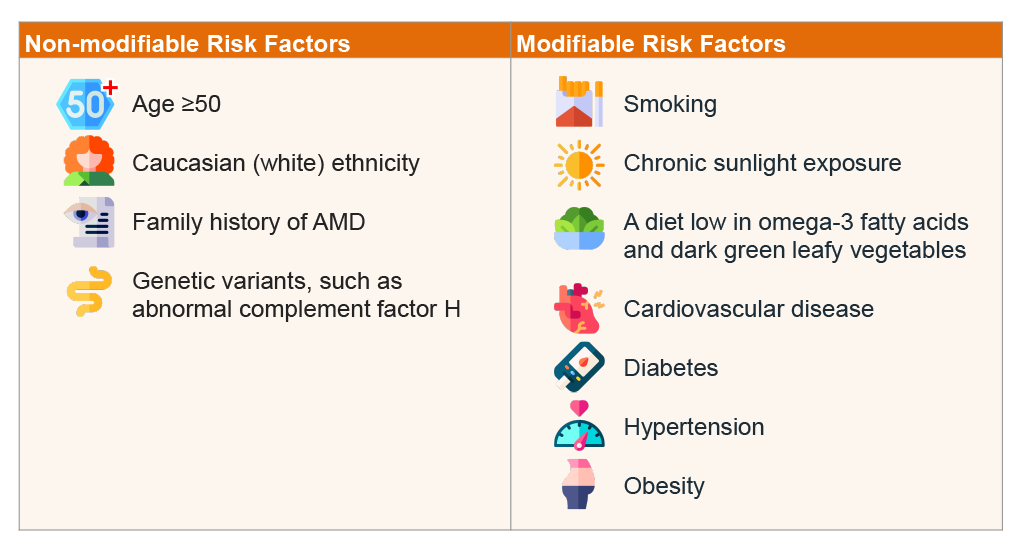
Risk factors for AMD
Common in older adults, age is the most significant risk factor for AMD, with the prevalence increasing with age.2–5
Smoking is the environmental factor that is most strongly associated with AMD, particularly neovascular AMD (nAMD), increasing the risk of atherosclerosis that can affect the choroidal vessels of the eye. Nicotine also promotes inflammation and angiogenesis through the upregulation of vascular endothelial growth factor (VEGF). Patients who smoke cigarettes are twice as likely to develop AMD as nonsmokers; however, quitting smoking can lower both the risk and severity of the condition.3,6,7,8
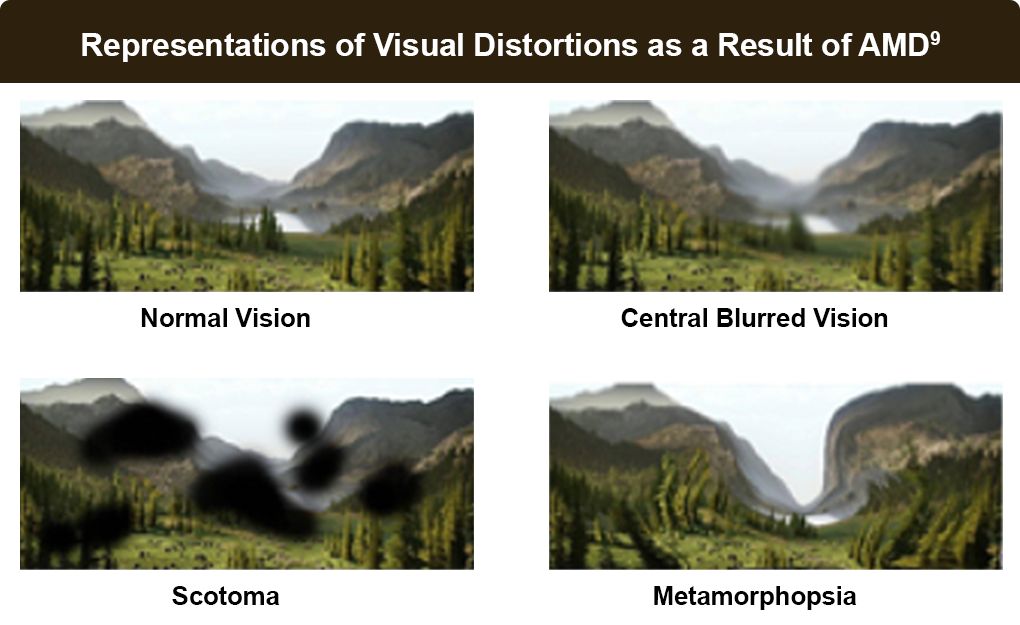
Symptoms of AMD
People at higher risk for AMD should have increased vigilance for symptoms of AMD to allow for earlier detection and treatment, which can offer improved outcomes.2,3,8 Symptoms of AMD include central blurring, metamorphopsia, decreased vision, scotoma, photopsia, colors appearing faded, and difficulties in dark adaptation, which can change as the disease progresses:2,3,6
- Early AMD is often not noticed by many people, other than noticing increasing difficulty seeing in low-light situations
- Intermediate AMD symptoms can include a blurry spot in the center of patient’s vision, perception of less intense colors or contrast sensitivity, and increasing difficulty in low light
- Advanced, or late-stage AMD, can present as worsening or distorted visual acuity, central vision loss, and difficulty in recognizing faces
Screening and monitoring for AMD
The American Academy of Ophthalmology (AAO) recommended frequency for adult comprehensive medical eye examinations for asymptomatic patients, and for patients who do not have risk factors for eye disease, is under 40 years–every 5 to 10 years; 40 to 54 years–every 2 to 4 years; 55 to 64 years–every 1 to 3 years; and 65 years or older–every 1 to 2 years.1
Patients at higher risk should be evaluated more frequently:1,2

Patients who are aged >60 years

Patients with hypertension or cardiovascular disease
Cigarette smokers
Patients with a history of AMD in first-degree family members
Patients with a history of significant cumulative light exposure
Patients with decreased dark adaptation or other symptoms consistent with AMD
Findings of macular drusen may be an incidental funduscopic finding that should prompt providers to refer patients with significant risk factors to an ophthalmologist.10
For a patient with AMD, more frequent retinal examinations are recommended, such as moving from a 12-month follow-up interval to a 6-month interval to monitor disease progression, or every 3-4 months for those who are progressing rapidly or at high risk for choroidal neovascularization (CNV).3
Patients with the onset of new symptoms, such as new visual loss, metamorphopsia, or scotoma, should be examined promptly. Any sudden loss of vision (days up to a week) should be evaluated within 48 hours; visual changes occurring over weeks to months should be assessed nonurgently at the next available appointment.3,10
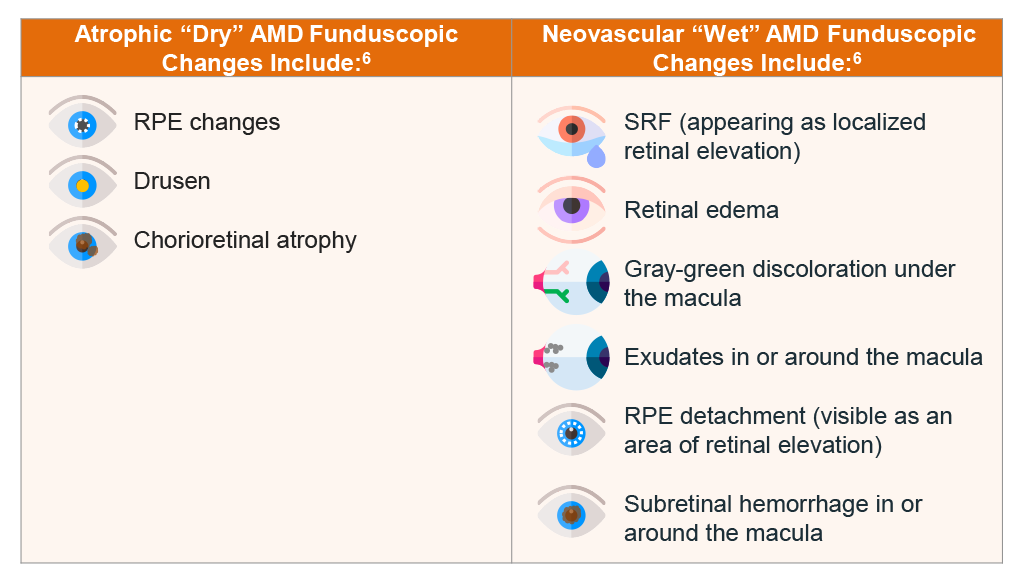
Making the diagnosis
The diagnosis of AMD usually is made clinically based on the patient’s history, symptoms, and a dilated eye exam using a binocular slit-lamp biomicroscopy of the ocular fundus to detect drusen, abnormalities in the retinal pigment epithelium (RPE), geographic atrophy (GA), CNV, subretinal fluid (SRF), and hemorrhage.6
Clinicians should obtain a thorough history for symptomatic patients to assess the onset of visual symptoms, whether one or both eyes are affected, and if the vision loss involves far vision, near vision, or both. The physical examination should include visual acuity, visual fields by confrontation, external eye and lid assessment, pupillary function, extraocular movement, and a funduscopic evaluation.10
An optometrist or ophthalmologist can use different imaging tests to assess, diagnose, and classify AMD, as well as to monitor treatment and disease progression.3,10,11
- Optical coherence tomography (OCT) is a noninvasive imaging technique that provides high-resolution, cross-sectional images of the retina, retinal nerve fiber layer, and the optic nerve head. OCT can be used to determine the presence of subretinal and intraretinal fluid and retinal thickening and is used to monitor progression and therapeutic responses to therapy in patients with nAMD. Home-based OCT scanning could be used to monitor disease. Optical coherence tomography angiography (OCTA) is becoming more commonly used in AMD. If offers noninvasive evaluation of the retinal and choroidal vasculature, and may detect subclinical CNV, which requires close monitoring and not treatment. progression and treatment efficacy, potentially alleviating some of the burden involved with managing AMD. Newer-generation OCT modalities offering faster scanning speeds and higher resolution are preferred, such as spectral domain OCT and swept-source OCT.3,10,11
- Fluorescein angiography should be performed on patients suspected of having choroidal neovascularization based on symptoms or findings on physical examination. This includes patients complaining of new metamorphopsia or unexplained blurred vision; those with findings of macular edema, subretinal blood, or elevation of the RPE on examination; or those with OCT-detected fluid. Patients being considered for treatment with either photodynamic therapy or laser photocoagulation should have angiography to guide therapy and to evaluate recurrences after treatment. The dye is injected intravenously as a bolus, and a sequence of photographs are taken. Newly formed choroidal vessels leak fluorescein that appears on imaging; normal retinal vessels do not.3,10,12
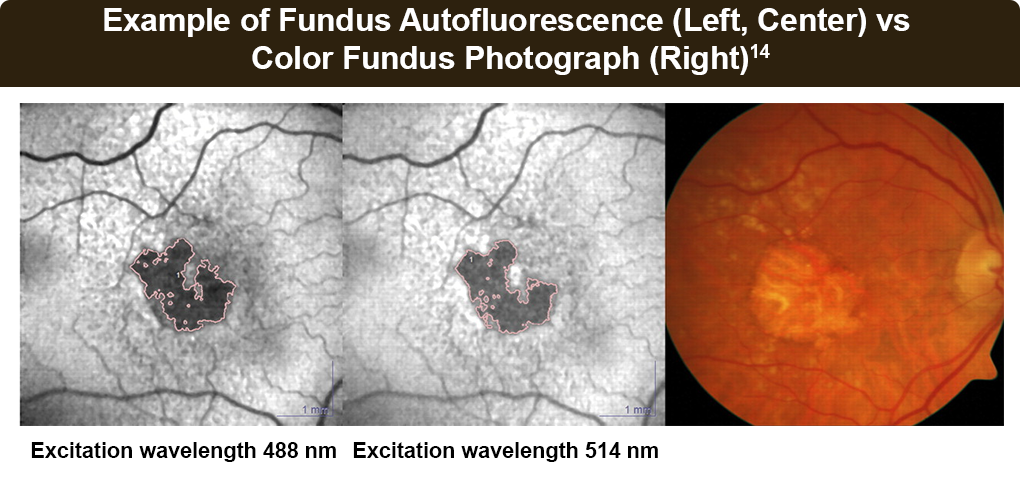
- Fundus autofluorescence (FAF) is a non-invasive imaging modality that can identify areas of geographic atrophy and can be used to monitor these areas for disease progression. This test also allows for identification of lipofuscin accumulation in the RPE. Atrophic RPE typically appears as dark patches in FAF, and some patterns may predict faster rates of geographic atrophy. Green-light FAF images may be superior to blue-light to accurately determine small, central, pathologic changes, and central atrophic lesion boundaries.3,10,13,14
- Indocyanine green angiography allows visualization of the choroidal circulation, shown to be useful in evaluating specific forms of AMD, such as PED, poorly defined or occult MNV, and lesions including retinal angiomatous proliferation or idiopathic PCV. Risks can include severe medical complications, allergic reactions, and death. Indocyanine green does not cross the placenta and is generally safe in pregnancy.
References
- Chuck RS, Dunn SP, Flaxel CJ, et al. Comprehensive Adult Medical Eye Evaluation Preferred Practice Pattern®. Ophthalmology. 2021;128:P1-P29.
- Centers for Disease Control (CDC). About Age-Related Macular Degeneration. Vision and Eye Health. May 21, 2024. https://www.cdc.gov/vision-health/about-eye-disorders/age-related-macular-degeneration.html
- Vemulakonda GA, Bailey ST, Kim SJ, et al. Age-Related Macular Degeneration Preferred Practice Pattern®. Ophthalmology. 2025;132(4):P1-P74.
- Mahmood S. Age-related macular degeneration – Symptoms, diagnosis and treatment | BMJ Best Practice US. BMJ Best Practice. May 29, 2024. https://bestpractice.bmj.com/topics/en-us/554
- Cavallerano A. Clinical Practice Guidelines: Care Of The Patient With Age-Related Macular Degeneration. Published online 2004. https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/Consensus-based%20guidelines/Care%20of%20the%20Patient%20with%20Age-Related%20Macular%20Degeneration.pdf
- Mehta S. Age-Related Macular Degeneration (AMD or ARMD) – Eye Disorders. Merck Manual Professional Edition. April 2024. https://www.merckmanuals.com/en-ca/professional/eye-disorders/retinal-disorders/age-related-macular-degeneration-amd-or-armd
- Kulkarni A, Banait S. Through the smoke: An in-depth review on cigarette smoking and its impact on ocular health. Cureus. 2023;15:e47779.
- Centers for Disease Control (CDC). Why Vision Loss Is a Public Health Problem. Vision and Eye Health. May 24, 2024. https://www.cdc.gov/vision-health/about-eye-disorders/vision-loss-public-health-problem.html
- The Eye Foundation. Diabetic Retinopathy and Macular Edema – Causes, Symptoms, and Treatments. https://www.theeyefoundation.com/diabetic-retinopathy-macular-edem
- Cunningham J. Recognizing age-related macular degeneration in primary care. JAAPA. 2017;30:18-22.
- Blinder KJ, Calhoun C, Maguire MG, et al. Home OCT imaging for newly diagnosed neovascular age-related macular degeneration: A feasibility study. Ophthalmol Retina. 2024;8:376-387.
- Domalpally A, Danis RP. Fluorescein Angiography in Neovascular AMD. Review of Ophthalmology. August 25, 2008. https://www.reviewofophthalmology.com/article/fluorescein-angiography-in-neovascular-amd
- Ruiz-Moreno J, Montero J, Ruiz-Medrano J. Fundus autofluorescence in age-related macular degeneration | amdbook.org. July 2017. https://amdbook.org/content/fundus-autofluorescence-age-related-macular-degeneration
- Wolf-Schnurrbusch UEK, Wittwer VV, Ghanem R, et al. Blue-light versus green-light autofluorescence: Lesion size of areas of geographic atrophy. Invest Ophthalmol Vis Sci. 2011;52:9497-9502.